Rates of syphilis, gonorrhea, and chlamydia infection have continued to rise, according to the Centers for Disease Control.
Both total numbers of infections and per capita rates of the three STDs continued their more-or-less uninterrupted climb since the turn of the millennium. In total, rates of infection are at their highest level since the CDC began tracking chlamydia infections in 1984.
![]()
Not all of this increase is attributable to an actual bump in the number of individuals infected. The CDC counts the number of positive tests reported to it by states, a figure which necessarily also increases as testing becomes more commonplace. Similar changes in the data can be caused by more states reporting or by improved testing practices. Still, recent increases between years—when testing practices have not dramatically changed—likely indicate an increase in the number of infections themselves.
To understand how America is being affected by this wave of STDs, it helps to look at each underlying STD individually.
![]()
Perhaps the easiest trend to explain is the almost uninterrupted rise in chlamydia. Increased testing, and the refinement of testing methods—the new report points to the expanded use of "nucleic acid amplification tests" between 2000 and 2011 in particular—likely play an outsized role in the spike. This conclusion is further supported by a separate CDC report which, relying on sequential random samples of the population, found that there was no statistically significant increase in the chlamydia rate between 1999 and 2012.
The report does, however, highlight the surprising prevalence of chlamydia, particularly among young, sexually-active women. Up to 4 percent of the female population ages 15 to 24 tests positive for the disease, compared to roughly 1 percent of men in the same age group and less than 1 percent of both men and women in other age groups. Chlamydia is generally asymptomatic in women, the report notes, meaning that many then act as unwitting carriers of the disease to male partners.
Syphilis and gonorrhea are less common, but both have experienced recent increases in prevalence. Rates of syphilis fell from a peak in 1990 to a historic low in the early 2000s, before creeping steadily back up in the past couple of decades. Gonorrhea infections increased by 82.6 percent since reaching a historic low in 2009.
Both increases appear to be concentrated among "men who have sex with men" (MSM, a stated-sexual-preference-neutral term used by the CDC and other public health organizations). MSM "continued to account for the majority of" primary and secondary syphilis diagnoses in 2018, a trend which appears to have been on-going since at least 2014.
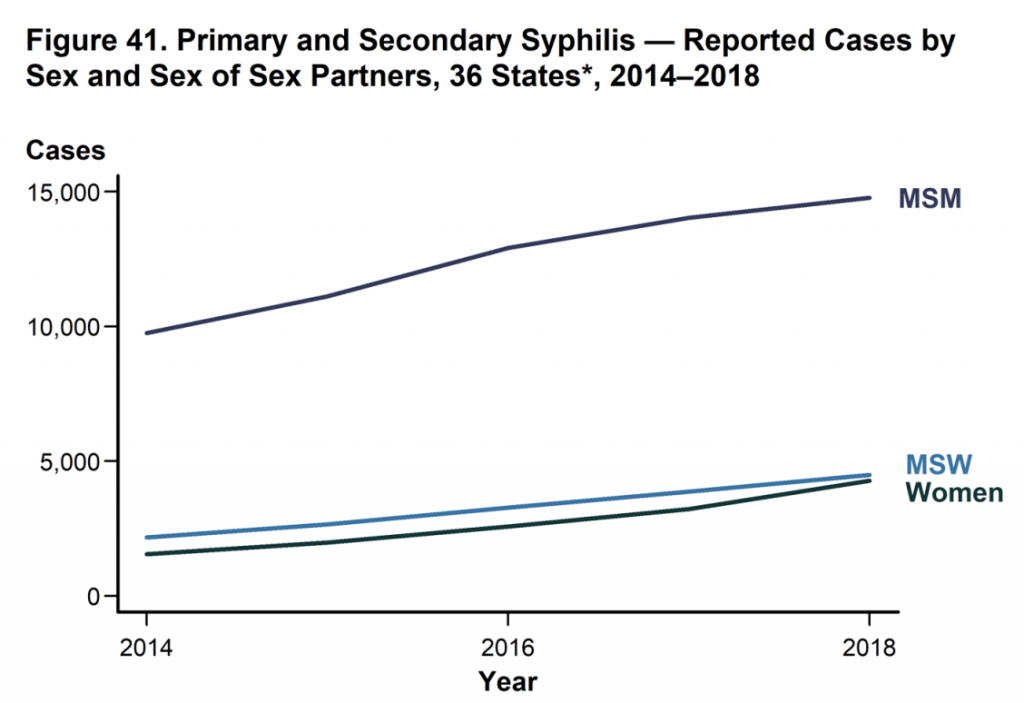
The same conclusion can be reached, albeit with less certainty, about gonorrhea. The CDC pointed to separate research, based on data from its STD Surveillance Network, which surveys STD sufferers. Those data, drawn from interviews in four cities and two states, suggest that by 2015 MSMs were 24 times likelier to have gonorrhea than women, and 31 times likelier than "men who have sex with women."
In a companion release, the CDC suggested that "multiple factors, including individual behaviors and sexual network characteristics," may determine the high prevalence of STDs among MSM. Those network characteristics included "high prevalence of STDs, interconnectedness and concurrency of sex partners, and possibly limited access to healthcare," as well as socioeconomic disadvantage among certain MSM subpopulations.
At the same time, rising rates of infection among a vulnerable subpopulation are not the only major health threats posed by STDs. The new report highlights a startling increase in syphilis among newborns. The number of reported cases of "congenital syphilis" has nearly tripled since 2014, rising to 1,306 in 2018. In general, an infected mother has an 80 percent likelihood of transmitting syphilis to her child.
The other major health risk mentioned by the report is the rise of antibiotic resistant gonorrhea. Although the first line of defense against gonorrhea, ceftriaxone, remains effective, the CDC found that more than half of all gonorrhea infections reported in 2018 were resistant to at least one antibiotic.
Why, then, are rates of STD infection increasing, particularly among vulnerable communities? The CDC suggested that "multiple factors" are at play, including "drug use, poverty, stigma, and unstable housing, which can reduce access to STD prevention and care," "decreased condom use among vulnerable groups," and "cuts to STD programs at the state and local level."
Working to reduce STDs—as the Trump administration is with HIV—will have major benefits, according to Dr. Jonathan Mermin, the director of CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention.
"STDs can come at a high cost for babies and other vulnerable populations," Mermin said. "Curbing STDs will improve the overall health of the nation and prevent infertility, HIV, and infant deaths."